Ankle Brachial Index: most useful screening test for peripheral arterial disease (simple, quick, non-invasive, done at bedside). This test should be performed in patients with one or more findings that are consistent with PAD on either review of systems or physical exam. ABI is the ratio of the ankle systolic blood pressure divided by the brachial systolic blood pressure that is detected using a Doppler probe. Normal ABI is measured at approximately 1-1.2, and a (+) finding for PAD would be ABI <0.90 (high degree of both sensitivity as well as specificity for PAD). It is important to note that a reading of >1.2 can be possibly due to non-compressible (calcified) vessels which can lead to a false reading
Duplex imaging: can be used to evaluate the vasculature preoperatively, intraoperatively and post-operatively and is extremely useful in identifying proximal arterial disease. It’s also non-invasive, and is often used when there is inability to palpate a given vessel in a patient with suspected PAD.
Arteriography: considered the gold standard for diagnosing PAD but its usually reserved for cases where revascularization is planned
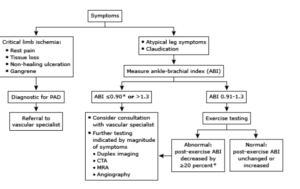
ALGORITHM (when to use what): if there are clear indications for critical limb ischemia (i.e. rest pain, gangrene, non-healing ulceration) then this is considered diagnostic for PAD and quick referral to vascular specialist is warranted. If the patient has atypical leg symptoms and claudication, the first step would be to measure their ABI, and if it was measured to be below 0.9 or above 1.3 further testing might be indicated if there is magnitude of symptoms (and included in those would be duplex imaging)
ALT: alanine aminotransferase AST: aspartate aminotransferase (both liver enzymes commonly measured in the serum). They are sensitive indicators of some form of liver cell injury. These enzymes catalyze the transfer of the alpha-amino groups of alanine and asparate respectively, to the alpha keto group of ketoglutarate which results in the formation of pyruvate and oxaloacetate.
Normally AST is found in a variety of tissues (i.e. liver, heart, muscle, kidney, brain) and is released into the serum when any one of those are damaged. For instance, AST level can be elevated in case of an MI or some form of muscle damage. Because of this, AST is not a highly specific indicator of liver injury since its elevation can be a result of other tissues being injured. AST is increased in AMI, liver disease, Reye syndrome, muscle trauma, pancreatitis, intestinal injury/surgery, burns, renal infarction, and certain medications. On the flip side, AST can be decreased in instances like Vitamin B6 deficiency (Beriberi), DKA, liver disease, and hemodialysis.
ALT on the other hand is normally found mostly in the liver. While it can be elevated due to injury elsewhere, majority is concentrated in the liver thereby making ALT a more specific test than AST for detecting liver injury. ALT is increased in liver disease, biliary obstruction, pancreatitis, and often in alcoholics.
The normal levels for AST and ALT are approximately 8-40 units/liter (give or take). Mild to moderate elevations are generally considered to less than 15x the upper limit of normal, which would indicate some form of mild injury or mild inflammation going on in the liver. If there is severe elevation where the value is up in the 1000s range then there is something more abnormal going on like concern for hepatitis, cirrhosis of the liver, liver damage from acetaminophen toxicity, or some cause of diminished blood flow to the liver (i.e. shock or heart failure). It is important to note that there can be certain instances where ALT/AST can be falsely elevated or decreased. For example drugs like Erythromycin and Furosemide can cause false elevations, while patients taking Isoniazid can have falsely low serum AST. Using just these aminotransferases alone are often of little prognostic value, and that is why they are often ordered in conjunction with other tests like bilirubin and alkaline phosphatase etc. to accurately determine the extent of liver failure.
- Amoxicillin/Clavulanate (Augmentin)
- I included this antibiotic because it is a combination of both amoxicillin (aminopenicillin) and clavulanic acid (beta lactamase inhibitor). It provides coverage for gram-positive cocci (MSSA, Streptococci), gram negative bacilli (E coli, P mirabilis, Klebsiella), as well as anaerobes. Augmentin is a commonly used antibiotic in both adults and children and is indicated for conditions such as otitis media, pneumonia, bacterial rhinosinusitis, UTI, etc.
- Azithromycin
- I included this antibiotic because it is a macrolide that is commonly used for a wide range of bacterial infections (i.e. respiratory, skin, GI, GU). It provides coverage for gram-positive cocci (MSSA, Streptococci), atypical organisms, and is often used as an alternative when a patient is allergic to Penicillin. Another benefit is the capability of Azithromycin to be prescribed to pregnant patients as well as those who are breastfeeding.
- Ceftriaxone
- I included this antibiotic because it is a third-generation cephalosporin that provides coverage for both gram positive cocci (MSSA, Streptococci) as well as gram negative bacilli (E coli, P mirabilis, Klebsiella, N gonorrhoeae, N meningitis). It is used for a wide range of bacterial infections such as pneumonia, meningitis, as well as gonococcal infections. Another benefit is that there are no documented severe interactions with other drugs, or absolute contraindications to its use (except for documented hypersensitivity to the drug/class).
- Piperacillin/Tazobactam (Zosyn)
- I included this antibiotic because it is a combination of an aminopenicillin with a beta lactamase inhibitor. It provides broad coverage of gram-positive cocci (MSSA, Streptococci) as well as gram negative bacilli (E coli, P mirabilis, Klebsiella), particularly Pseudomonas and anaerobic coverage. Zosyn is indicated for the use of intra-abdominal infections, gynecologic infections, skin infections, amongst others, thereby making it a useful antibiotic across many specialties.
- TMP/SMX (Bactrim)
- I included this antibiotic because it is a nitroimidazole that is a combination of two antibiotics (sulfamethoxazole and trimethoprim). It provides broad coverage of gram-positive cocci (MSSA, Streptococci) including MRSA, gram negative bacilli (E coli, P mirabilis, Klebsiella) including ESCAPPM (pneumonic for gram negative rods that are multi-resistant), as well as N meningitis. Bactrim is indicated for the use of many bacterial infections and is used as both treatment and prophylaxis for PCP (pneumocystis carinii pneumonia) and Toxoplasmosis, making it a particularly useful antibiotic for HIV patients.


