Acute Pericarditis: inflammation of the pericardium (outer layer of heart)
~2 most common causes are either idiopathic or viral (Coxsackievirus & Echovirus)
~Typical presentation is a sudden onset of pleuritic chest pain (sharp, worse with inspiration) that is persistent, postural (worse when supine but improved by leaning forward).
~This pain can radiate to the shoulder, back, neck, arm or even epigastric area
~Pericardial friction rub is a classic clinical feature [hear a superficial scratchy or squeaky sound using the diaphragm of the stethoscope over the left sternal border]
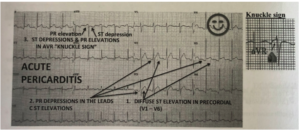
~EKG: see diffuse ST elevations in the precordial leads (V1-V6) with associated PR depression in those leads [PANCE PREP PEALRS PIC]; see the opposite in aVR (PR elevations, ST depressions)–> “knuckle sign”
~Echo: useful to see if there is evidence of pericardial effusion or signs of cardiac tamponade but often times its normal for a patient with this condition
~Labs: pericarditis= inflammatory disease so you’ll see elevated white count, ESR, CRP, but they’re not sensitive/specific for pericarditis
~Patients who are “high risk” need to be admitted [fever above 100.4, subacute course, large pericardial effusion, immunosuppression, acute trauma, elevated cardiac troponin, etc.] vs. lower risk can be treated as outpatient
~Regardless, nearly all patients are going to receive NSAIDs along with Colchicine as 1st line for 7-14 days (symptoms should start to subside in 1-2 days). Patient should also be advised to restrict from any strenuous activity. If the patient is responding to therapy, for long term management: taper the NSAIDs and complete 3 months of colchicine therapy & arrange for follow up.
~Dressler syndrome (post MI pericarditis): aspirin or colchicine; need to avoid NSAIDs because interfere with myocardial scar formation
Hypertrophic Cardiomyopathy:
~autosomal dominant genetic disorder of inappropriate left ventricular and/or right ventricular hypertrophy with diastolic dysfunction
~most common cause of sudden cardiac death in young athletes young athlete patient with family history of sudden cardiac death [usually due to v-fib]
~most common symptom is dyspnea; also see fatigue, angina (chest pain), pre-syncope, syncope, dizziness, arrythmias, but patient can also be asymptomatic initially
~on physical exam you’re going to hear a harsh systolic murmur at the left sternal border; the murmur will become more intense if there is a decrease in venous return or afterload [Valsalva maneuver or standing]; vs. the murmur becoming less intense when there is increased venous return or afterload [squatting, supine]
~Echocardiogram is used to establish the diagnosis see asymmetric ventricular wall thickness (especially septal wall) measured at 15mm or greater; also see systolic motion of the mitral valve, and small LV chamber size
~EKG: evidence of left ventricular hypertrophy, anterolateral and inferior pseudo q waves, enlarged atria
~Tx: want to try and detect it early and can be managed either medically, surgically, or with the placement of ICD
*Medical: beta blockers= first line [also use CCBs]
*Surgical: myomectomy usually performed in young patients that are refractory to medical Tx
~Overall need to advise patients to avoid dehydration, extreme exertion, exercise; Also should be cautious in using Digoxin (increases contractility) Nitrates & Diuretics (decrease LV volume)


